According to Hipaa Regulations Which of the Following May Reduce
For hardcopies this typically involves shredding or pulping. This opens the door to a number of security issues covered by the HIPAA Security Rule to prevent such things as ransomware attacks identity theft and malicious behavior ie.

New Updates In Hipaa Regulations For 2021
This is a summary of key elements of the Security Rule including who is covered what information is protected and what safeguards must be in place to ensure appropriate protection of electronic protected health information.

. May 21 2008 and the Health information Technology for Economic and Clinical Health HITECH Act Pub. Because it is an overview of the Security Rule it does not address every detail of. For ePHI the disposal process could involve degaussing secure wiping or destruction of the portable device on which the ePHI is stored.
The HIPAA Breach Notification Rule. In addition the Department of Health and Human Services HHS may upon specific request from a State or other entity or person determine that a provision of State law which is contrary to the Federal requirements as defined by the HIPAA Administrative Simplification Rules and which meets certain additional criteria will not be. Technology has made information sharing easier than ever but it also comes with risks.
Summary of the HIPAA Security Rule. Unique Identifiers Rule National Provider Identifier NPI HIPAA-covered entities such as providers completing electronic transactions healthcare clearinghouses and large health plans must use only the National Provider Identifier NPI to identify covered healthcare providers in standard transactions. As a result theres no official path to HIPAA certification.
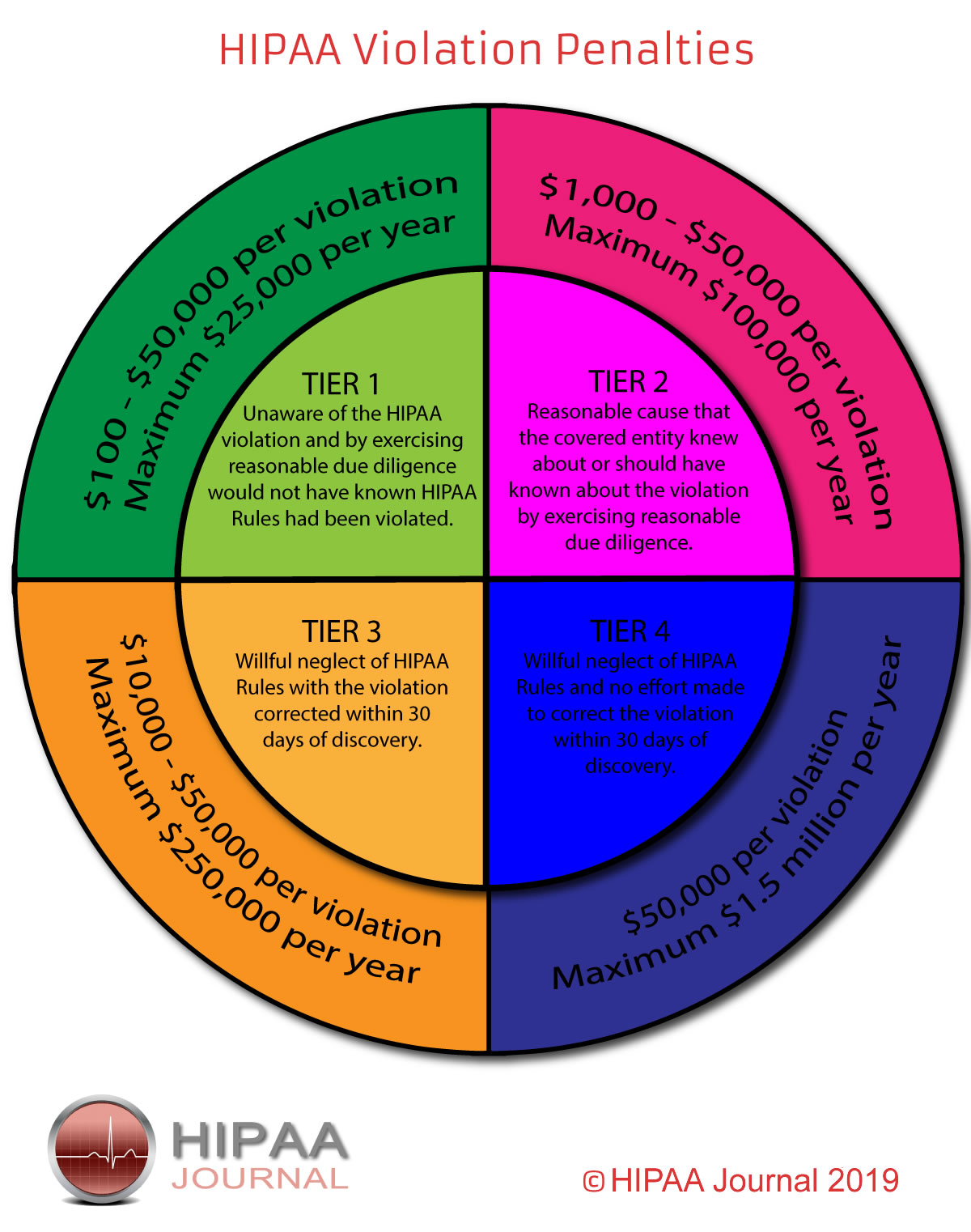
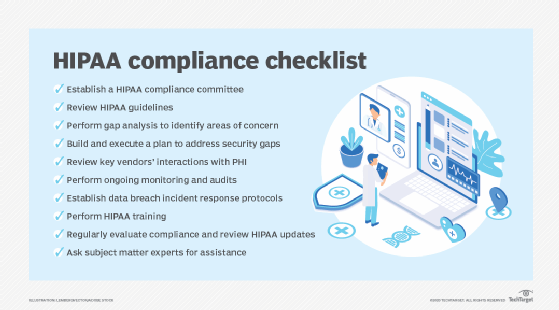
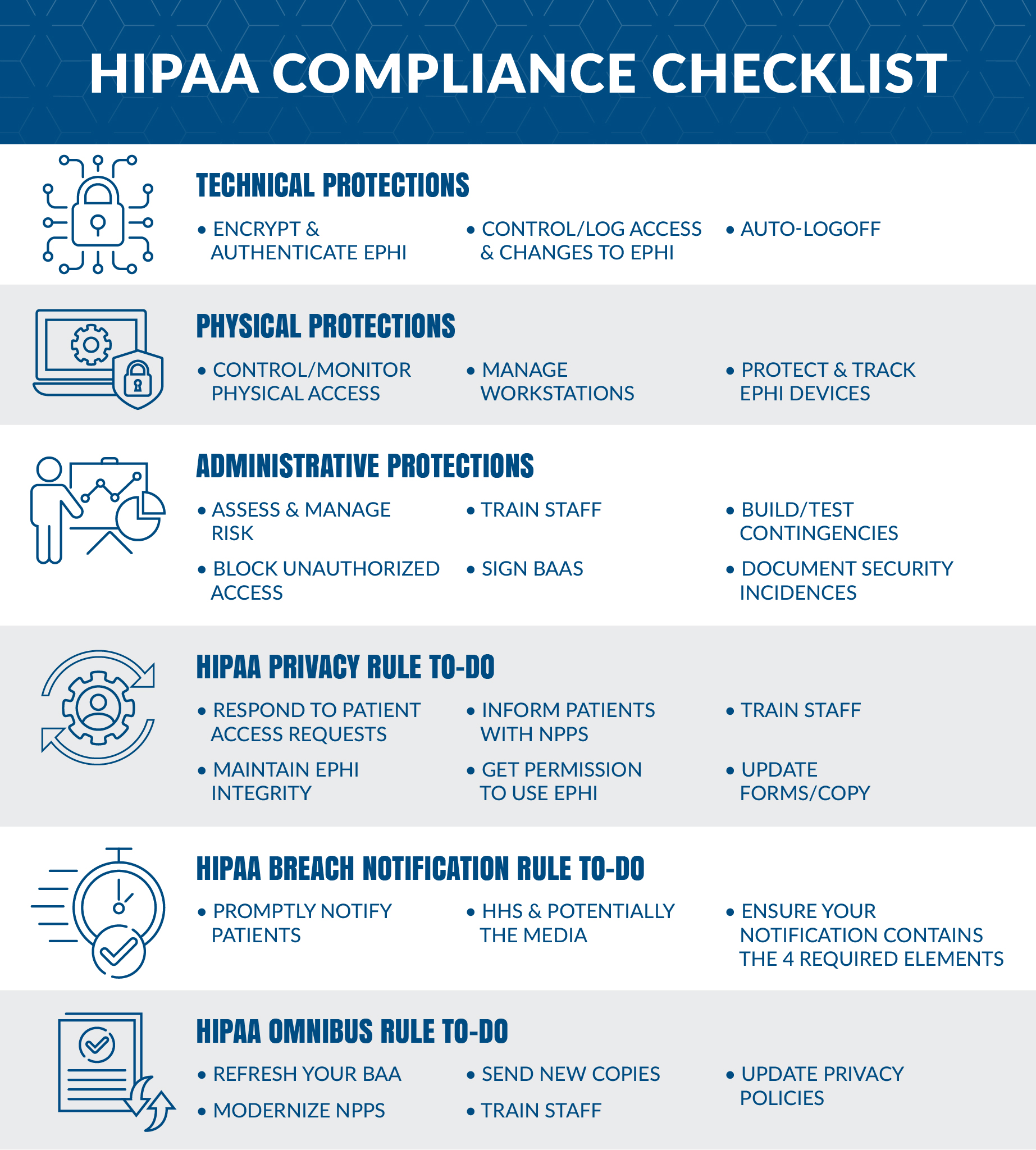
An essential feature of HIPAA it allows for extended health insurance coverage for employees when they are between jobs or switching employers. 226 February 17 2009. Our HIPAA security rule checklist explains what is HIPAA IT compliance HIPAA security compliance HIPAA software compliance and HIPAA.
Kim is covered under two medical expense plans. Anyone working in a medical facility D. 2 See also the HIPAA Security Rule 45 CFR Parts 160 and 164 Subparts A and C the HIPAA Breach Notification Rule 45 CFR Part 164 Subpart D and the HIPAA Enforcement Rule 45.
HIPAA does not regulate the price of health insurance but rather it relies on tax breaks and other tax incentives to reduce health care costs Chaikind et al. Only attending healthcare workers who do direct patient care B. Everything you need in a single page for a HIPAA compliance checklist.
Plan B pays up to 4000. Today earning HIPAA certification is a part of due diligence. Among the most common examples of business associates are billing companies practice management firms third.
The law refers to these as covered entities. If your organization has access to ePHI review our HIPAA compliance checklist for 2021 to ensure you comply with all the HIPAA requirements for security and privacy. An attorney receives the wrong patients information via fax Which of the following must comply with HIPAAs requirements to protect the privacy and security of health information.
Through careful policies HIPAA lowers the risk of fraud and abuse to both the patient and the health care provider. Plan A pays up to 5000 and Plan B pays up to 2000. Frequently Asked Questions for Professionals - Please see the HIPAA FAQs for additional guidance on health information privacy topics.
According to HIPAA regulations both physical and electronic PHI must be properly disposed of after their retention periods have expired. Plan A pays up to 5000. Most health care providers including doctors clinics hospitals nursing homes and pharmacies.
Ensuring that employees home offices comply with HIPAA rules will significantly reduce the risk of a data breach as well as the organizations liability in the event of a compliance violation. Libel slander defamation of character And while HIPAA does not allow affected patients to sue covered entities CE in response to a mishandling of PHI healthcare laws vary by state and. Employer and insurance company.
An _____ is a detailed document that describes the protected health information to be used and disclosed the person authorized to make the use or disclosure the person to whom the covered entity may make the disclosure an expiration date and in some cases the purpose for which the information may be used or disclosed. Within ten days of hire new employees must complete an OSHA training program. With HIPAA certification you can prove that your staff members know how to comply with HIPAA regulations.
The following entities must follow The Health Insurance Portability and Accountability Act HIPAA regulations. Topics range and may consist of protective equipment medical waste management information following an exposure control plan reducing the risk of exposure handling hazardous chemicals and how to deal with other workplace hazards. The HIPAA Breach Notification Rule requires Covered Entities and Business Associates to report when unsecured PHI has been acquired accessed used or disclosed in a manner not permitted by.
Nurses are busy and often it is easiest to catch a colleague or caregiver in passing to relay patient information. Which of the following may NOT be considered incidental to a permitted use or disclosure. Work from Home Policy for Healthcare Employees A work from home policy for healthcare employees is crucial to mitigating the risk of a data breach.
Only the billing department C. HIPAA compliance rules change continually. If she incurs 7000 in expenses the coordination of benefits provision dictates that.
The version issued in 2006 has since been amended by the HITECH Act in 2009 and the Final Omnibus Rule in 2013. Make every effort possible to control the environment to reduce the risk of HIPAA violations. HIPAA regulations define business associates as people or organizations that perform specific functions or activities handling transmission and processing that involve the use of the PHI or provide services to some of the covered entities.
A visitor who asks for a patient by name. HIPAA security and privacy regulations apply to. A group health insurance policy is a contract between an.
0 Response to "According to Hipaa Regulations Which of the Following May Reduce"
Post a Comment